TMS for the Developing Brain: New Evidence in Adolescent Depression
When a teenager is struggling with depression, families are often forced to navigate uncertainty—about treatment options, timelines, and what comes next. While therapy and medication remain important tools, they are not the only evidence-based options available to adolescents today.
In December 2025, a landmark study published in JAACAP Open added important clarity to this conversation. The findings confirm what a growing body of research has been showing: Transcranial Magnetic Stimulation (TMS) is a safe and effective treatment option for adolescents and young adults with major depressive disorder.
For families seeking clear, research-backed guidance, this study represents a meaningful step forward.
Breaking News: What This Study Adds to the Evidence
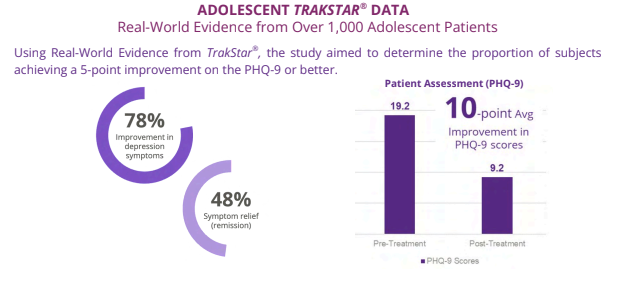
The study—led by Dr. Paul Croarkin and colleagues, leaders in pediatric mood disorders and neuromodulation—examined real-world outcomes of TMS in adolescents and young adults diagnosed with major depressive disorder.
Croarkin et al. (2025) reported that:
- Adolescents receiving TMS experienced significant reductions in depressive symptoms
- The treatment was well tolerated, with a safety profile consistent with what is seen in adults
- No age-specific safety concerns emerged
- Clinical improvement was observed across a range of treatment histories
Importantly, this research reinforces that TMS is not experimental care for teens—it is a scientifically grounded treatment with a growing and rigorous evidence base.
TMS for Teens: Not Just “After Everything Else Fails”
One common misconception is that TMS is only considered after every medication option has been exhausted. In reality, TMS is FDA-approved as an adjunctive treatment for adolescent depression, meaning it can be thoughtfully integrated earlier alongside therapy and, when appropriate, medication.
At New Chapter TMS, we’ve written about this in our Rooted in Research series, emphasizing that treatment planning should be individualized—not delayed by outdated assumptions about sequencing.
For many teens, TMS can:
- Reduce symptom burden earlier
- Improve engagement in therapy and school
- Avoid the need for repeated medication trials with limited benefit
Why the Developing Brain May Be Especially Responsive
Adolescence is marked by heightened neuroplasticity—the brain’s ability to adapt, reorganize, and form new connections. While this plasticity can increase vulnerability to depression, it also creates an opportunity for targeted, noninvasive neuromodulation.
TMS stimulates the left dorsolateral prefrontal cortex (DLPFC), a region involved in mood regulation, motivation, and executive functioning. Functional imaging studies show that this region often functions differently in depression, including in adolescents.
Repeated stimulation helps strengthen communication between the DLPFC and deeper emotion-processing networks, supporting more stable mood regulation over time.
This is one reason researchers and clinicians alike are paying close attention to how neuromodulation fits into adolescent mental health care.
How This Study Fits With the Broader Research Landscape
The Croarkin et al. findings build on a growing body of peer-reviewed research over the past five years:
- Wall et al., 2023 – Journal of Child and Adolescent Psychopharmacology
Demonstrated symptom improvement and good tolerability of rTMS in adolescents. - Dalhuisen et al., 2024 – The Lancet Psychiatry
Highlighted neuromodulation as an important component of modern depression treatment algorithms. - Sun et al., 2024 – Frontiers in Psychiatry
Reported safety and effectiveness of individualized TMS protocols in adolescents.
Taken together, the message is consistent: TMS is becoming an established, evidence-based option in adolescent depression care—not a fringe intervention.
Leadership in Adolescent TMS: Local Care, National Conversation
At New Chapter TMS, adolescent care is not a side offering—it is a core focus.
We are proud to be the most experienced provider of adolescent TMS for depression in the Spokane and Coeur d’Alene region, with no waitlist and a care model designed specifically for teens and young adults.
Dr. Kiira Tietjen (our founder and clinical director) brings:
- 10 years of experience as a psychiatric nurse practitioner
- A clinical background heavily focused on children, adolescents, and young adults
- Leadership roles in building adolescent intensive outpatient programs, including RISE and Charlie Health
Beyond local care, we are connected to the broader adolescent TMS field: Dr. Tietjen serves on a Clinical TMS Society (CTMSS) adolescent special interest panel alongside Dr. Croarkin and has participated as a Key Opinion Leader in national TMS panels alongside researchers including Drs. Hutton and Pages—all are co-authors of the JAACAP Open study.
This connection ensures that families in our region benefit not only from compassionate care, but from current, research-informed practice shaped by national collaboration.
Looking Ahead—With Care and Caution
While research continues to evolve—including ongoing work exploring optimized and accelerated protocols for adolescents—the core message remains clear:
Evidence-based TMS is already here, already safe, and already helping teens.
For families navigating adolescent depression, this study offers reassurance that effective, noninvasive options exist—and that they don’t have to leave the region to access them.
If you’re exploring whether TMS may be appropriate for your teen, our team is here to answer questions, coordinate with existing providers, and help you make an informed decision grounded in science.
👉 Contact New Chapter TMS to schedule a consultation or learn more about adolescent TMS care in Spokane and North Idaho.
Selected References
- Croarkin, P. E., et al. (2025). The Effectiveness of Transcranial Magnetic Stimulation in Adolescents and Young Adults With Major Depressive Disorder. JAACAP Open, 3(4), 1246–1258.
- Wall, C. A., et al. (2023). Adjunctive rTMS in adolescents with depression. Journal of Child and Adolescent Psychopharmacology.
- Dalhuisen, I., et al. (2024). Optimizing treatment strategies for depression. The Lancet Psychiatry.
- Sun, Y., et al. (2024). Individualized rTMS for adolescent depression. Frontiers in Psychiatry.