TMS for Teen Depression
A Safe, FDA-Approved Option
Depression in teenagers is more common than many people realize, and it can disrupt school, friendships, and family life. Parents often ask: “What happens if medication or therapy aren’t enough?”
The encouraging news is that Transcranial Magnetic Stimulation (TMS) is now FDA-approved for adolescents ages 15–21 with depression. Even more importantly, unlike in adults where TMS is typically a later option, the FDA approved TMS for teens as a first-line adjunct treatment.
That means teens don’t need to fail multiple medications before accessing TMS. It can be introduced alongside a first antidepressant or psychotherapy, much earlier in the treatment process.
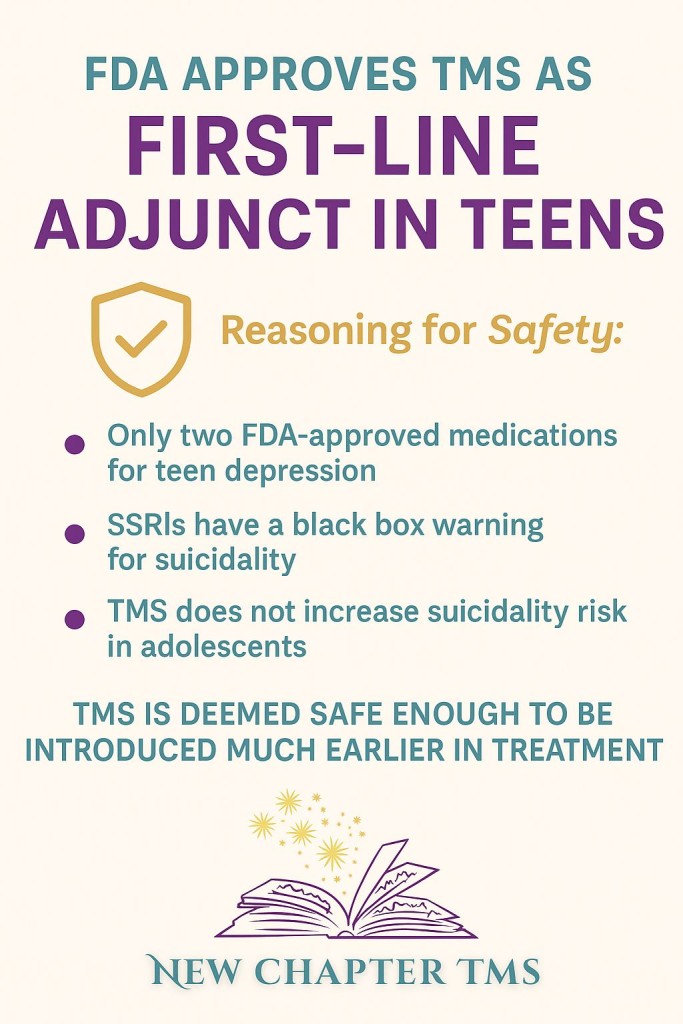
Why Did the FDA Approve TMS for Teens as ‘First Line Adjunct’?
There are unique considerations when treating adolescent depression:
- Limited medication options: Only two antidepressants are FDA-approved for teens.
- Black box warning on SSRIs: All antidepressants in this age group carry a warning about potential risk of increased suicidal thoughts.
- Proven safety of TMS: Clinical studies show that TMS does not increase suicidality in adolescents, making it a reassuring option for families.【1】【2】
The FDA’s decision reflects a balance of risks and benefits: TMS is safe enough to be used much earlier in a teen’s care plan.
Is TMS Safe for Teens?
Yes. TMS has been studied in thousands of patients worldwide, including adolescents, and has a very favorable safety profile.
- The most common side effects are mild scalp discomfort or headache, which usually improve after the first few treatments.
- No memory loss or cognitive side effects are associated with TMS.
- Teens remain awake and alert during treatment and can return to school or activities right after their session.
Why Early Access to TMS Matters
Depression during adolescence can derail education, friendships, and self-confidence. When depression lingers untreated, it increases risk of academic failure and suicidal thoughts.
By allowing TMS earlier, families now have a safe, evidence-based treatment option before months or years of ineffective medication trials. This can make a life-changing difference during a critical stage of brain development.
What Families Should Know
- Treatment plan: TMS is typically given 5 days per week for about 7 weeks.
- Insurance coverage: Many insurance plans now cover TMS for teens, though requirements vary by provider.
- Team approach: TMS works best when combined with therapy, school support, and family involvement.
Our Commitment at New Chapter TMS
At New Chapter TMS, this is more than just a treatment option — it’s our passion. Our founders, Dr. Kiira Tietjen and Will Normington, have decades of experience caring for acutely mentally ill teenagers in hospital and community settings. We’ve seen firsthand how depression can steal away a teen’s potential, and we’re deeply committed to offering safe, effective solutions like TMS to restore hope.
Frequently Asked Questions About Teen TMS
Does TMS replace medication or therapy?
No — TMS is usually added to ongoing treatment. It can be combined with therapy and sometimes with medication, depending on the care plan.
Will TMS change my teen’s personality?
No. TMS helps relieve symptoms of depression but does not change who your teen is.
Is TMS covered by insurance for teens?
Most major insurers now recognize adolescent TMS coverage. Our team helps with prior authorization and paperwork to make the process easier.
Key Takeaway
TMS is no longer just for adults. For teens, the FDA has recognized it as a first-line adjunct treatment because of its proven safety and effectiveness. If your teen is struggling with depression, TMS may be an important next step toward healing.
References
- U.S. Food and Drug Administration. Transcranial Magnetic Stimulation (TMS) – Expanded Indication for Adolescents (2022).
- Wall CA, et al. “Safety and tolerability of TMS in adolescents with depression.” J Child Adolesc Psychopharmacol. 2023.