Is TMS the Same as Shock Therapy? (No, Here’s Why)
If you’ve ever heard of “shock therapy,” you might wonder if Transcranial Magnetic Stimulation (TMS) is the same thing. The short answer: no, not at all.
This confusion is common — even among healthcare providers. But understanding the difference matters, because mixing them up keeps people from accessing safe and effective treatment for depression.
What Is ECT (“Shock Therapy”)?
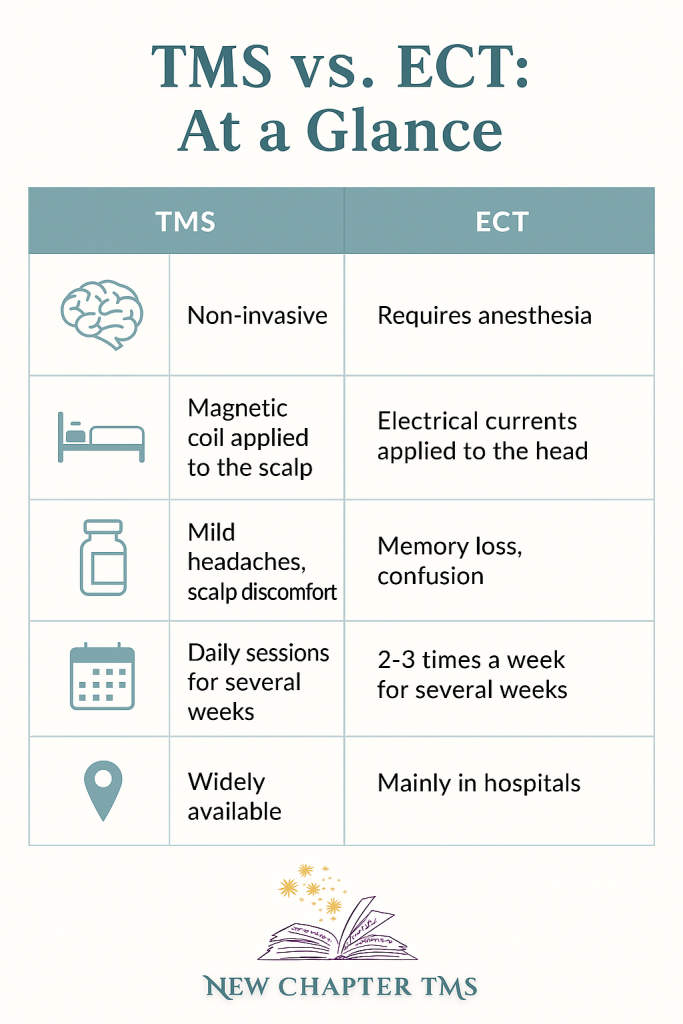
Electroconvulsive Therapy (ECT) has been used for severe depression since the 1930s. It does involve electricity. Patients are under anesthesia, electrodes are placed on the scalp, and a brief controlled seizure is triggered.
- Setting: Hospital or surgery center
- Anesthesia: Required
- Side Effects: Short-term memory loss, confusion, sometimes longer-term memory concerns
- When Used: Typically for very severe depression, psychosis, or when rapid response is needed (e.g., high suicide risk)
ECT can be life-saving, but it’s more invasive and comes with higher risks and side effects.
What Is TMS?
Transcranial Magnetic Stimulation (TMS) is completely different. Instead of electricity, TMS uses a magnetic field (similar to an MRI machine) to gently activate brain circuits involved in mood regulation.
- Setting: Outpatient clinic (you sit in a chair, awake the whole time)
- Anesthesia: Not required — you can drive yourself home after treatment
- Side Effects: Most commonly mild scalp discomfort or headache; no memory loss
- When Used: Depression that hasn’t improved with medications or therapy; also FDA-approved for teens (15–21) and for OCD
You can think of TMS as “physical therapy for the brain” — it strengthens underactive mood circuits over a series of sessions.
Why the Confusion?
Both ECT and TMS affect the brain, but that’s where the similarity ends. Because ECT has been around much longer, people sometimes assume all brain stimulation = shock therapy. Unfortunately, this leads to unnecessary fear and delayed treatment.
Recent research confirms that TMS is safe, effective, and very well tolerated — without the memory risks associated with ECT.
Quick Side-by-Side Comparison
Why This Matters
- Patients & Families: If you’ve tried multiple medications without success, TMS is a safe next step — not “shock therapy.”
- Teachers & Counselors: When supporting a struggling teen, know that TMS is FDA-approved and available locally.
- Providers: Don’t let outdated assumptions keep patients from care. TMS is evidence-based, covered by insurance, and should be in treatment plans.
References
- Perera T, George MS, Grammer G, Janicak PG, Pascual-Leone A, Wirecki TS. The Clinical TMS Society Consensus Review and Treatment Recommendations for TMS Therapy for Major Depressive Disorder. Brain Stimulation. 2016;9(3):336-346. (landmark consensus)
- Carpenter LL, et al. Transcranial magnetic stimulation (TMS) for major depression: A multisite, naturalistic, observational study of acute treatment outcomes in clinical practice. J Affect Disord. 2021;282:85-93.
- McClintock SM, et al. Consensus Recommendations for the Clinical Application of Repetitive Transcranial Magnetic Stimulation (rTMS) in the Treatment of Depression. J Clin Psychiatry. 2018;79(1):16cs10905.
- Milev RV, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2023 Clinical Guidelines for the Management of Adults with Major Depressive Disorder. Can J Psychiatry. 2023;68(9):609–639.